How AI Agents Reduce Provider Credentialing from 120 Days to 30 - Without Compromising Quality
Post Summary
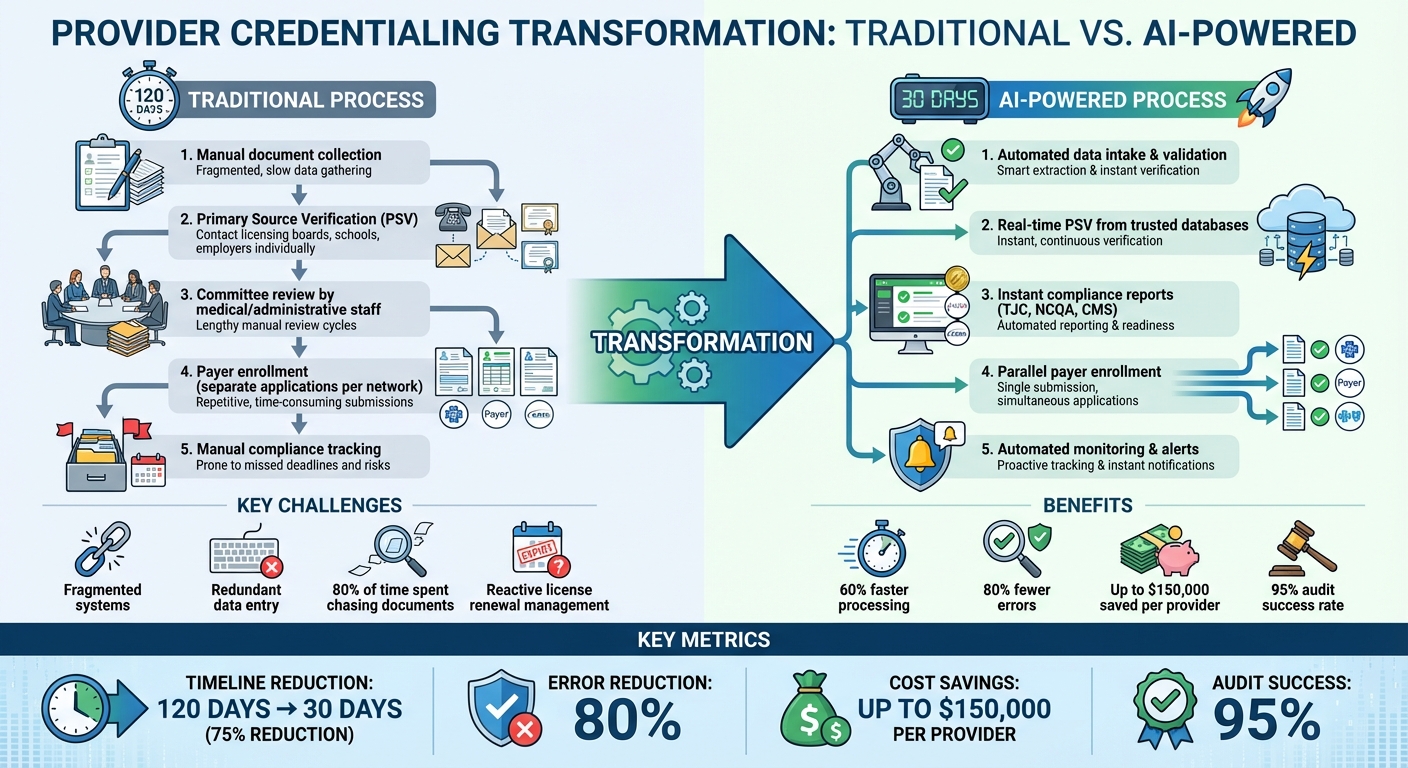
AI is transforming provider credentialing, cutting timelines from 120 days to just 30 without sacrificing accuracy or compliance. By automating manual tasks like document verification and data entry, healthcare organizations can onboard providers faster, reduce errors, and save money. Here’s how:
- Traditional Process: Manual steps like primary source verification (PSV) and payer enrollment stretch timelines to 120 days.
- Key Challenges: Delays stem from fragmented systems, redundant data entry, and compliance bottlenecks.
- AI Solutions: Automate PSV, flag inconsistencies, and sync data in real-time for faster, more reliable workflows.
- Results: 60% faster processing, 80% fewer errors, and up to $150,000 saved per provider by reducing delays.
This shift not only speeds up credentialing but ensures compliance and quality through a mix of automation and human oversight.
Traditional vs AI-Powered Provider Credentialing: 120 Days to 30 Days
The Standard Credentialing Workflow and Where It Slows Down
What Is Provider Credentialing?
Provider credentialing is the structured process healthcare organizations use to confirm a provider’s qualifications before they can care for patients or bill insurance. This involves verifying key professional credentials and background information. A vital part of this process is primary source verification (PSV), where licensing boards, educational institutions, employers, and other entities are contacted directly to confirm the authenticity of credentials [1][5]. Beyond PSV, credentialing also includes privileging (determining the procedures a provider is allowed to perform), payer enrollment (registering providers with insurance networks), and ongoing monitoring for license renewals and compliance [6].
Breaking down these requirements helps explain why the traditional process can take up to 120 days.
The 120-Day Workflow: Step by Step
Credentialing timelines, which often stretch between 60 and 120 days, are slowed by numerous manual steps [5]. Specialists must first gather provider documents and verify each one individually through PSV, contacting licensing boards, schools, and employers. Once this step is complete, the application undergoes committee review by medical and administrative staff. Only then does payer enrollment begin, requiring separate applications and verifications for each insurance network. Manual tracking of license renewals and compliance deadlines in disconnected systems further drags out the process [6].
These layers of complexity set the stage for the delays outlined below.
What Causes Delays
Delays in credentialing often stem from fragmented systems and inconsistent data. For example, health plans may receive large data files from delegated groups containing discrepancies - such as minor differences in address formatting ("St." vs. "Street") or missing NPI numbers - that slow down verification [2]. Outdated legacy systems and siloed data also lead to redundant data entry, which compounds inefficiencies [2].
"Before we implemented AI-assisted credentialing, I spent roughly 80% of my workday just chasing down documents and verifying information. It was like being a detective, but with much more paperwork." – Micah Schultz, credentialing specialist at a large medical group in Boston [5]
Manual processes introduce risks such as incorrect expiration dates or missing information, which can create compliance issues and lead to time-consuming rework [1][5]. Another challenge is the reactive nature of traditional credentialing, which often leaves specialists scrambling to manage license renewals at the last minute [5]. On top of that, varying state regulations, payer-specific requirements, and unique cases add more layers of complexity, further delaying the process [2][3].
Addressing these delays is crucial for improving efficiency, and this is where AI-powered solutions can make a significant impact.
How AI Enables a 30-Day Credentialing Process
AI transforms credentialing from a slow, manual task into a fast and automated system. Instead of spending weeks waiting for responses from licensing boards or manually entering data, AI instantly pulls and verifies information from trusted sources and multiple databases [1]. This shift removes the delays that used to stretch credentialing timelines to 120 days, replacing them with smooth workflows that maintain accuracy while significantly cutting down processing time.
The key to this speed lies in real-time data syncing and automated verification. AI-powered tools handle tasks like primary source verification, track responses, and flag inconsistencies as they happen - stopping errors before they lead to compliance problems. By integrating directly with HR systems, EHRs, and insurance reimbursement platforms, AI creates a unified workflow. This eliminates duplicate data entry and ensures consistency across systems. As a result, credentialing specialists can focus on handling exceptions that need human oversight. This automation paves the way for a streamlined process that completes in just 30 days.
What a 30-Day Process Looks Like
In a 30-day credentialing process, data quality takes center stage through automated intake and validation. Once documents are submitted, AI extracts the necessary data, checks for formatting consistency, and flags any missing information - sending immediate alerts for action. This upfront validation eliminates the back-and-forth delays that often slow things down.
AI systems verify credentials by pulling data from licensing boards, educational institutions, and malpractice databases in seconds. Instead of waiting on manual responses, these systems generate real-time compliance reports, tracking progress against federal, state, and accreditation standards like TJC, NCQA, and CMS. This ensures high-quality documentation while speeding up committee reviews. With pre-verified documents in hand, medical staff can focus on clinical privileging decisions rather than administrative tasks.
Payer enrollment happens alongside verification instead of after it. AI maintains centralized records that automatically populate payer applications across various insurance networks. This parallel processing, combined with ongoing monitoring for license renewals and compliance deadlines, compresses a process that used to take 120 days into a streamlined 30-day cycle. With every step optimized, performance metrics now provide a clearer picture of efficiency improvements.
Metrics to Track Progress
To measure success, track metrics like the average number of days for credentialing, the percentage of applications completed on the first review, time spent on manual data entry, response times for compliance alerts, and provider satisfaction. These indicators help evaluate whether AI-driven automation is delivering the speed and quality needed.
What AI Agents Do in Provider Credentialing
AI agents streamline the credentialing process by handling tasks with precision and efficiency.
Document Intake and Data Extraction
When documents come in, AI agents jump into action by pulling out key details like provider names, license numbers, and expiration dates. If any information is missing or unclear, the system flags it right away, cutting down on potential delays. This automated approach not only saves time but also sets the stage for quicker primary source verification.
Automated Primary Source Verification (PSV)
AI agents take on the heavy lifting of primary source verification by directly accessing trusted federal databases. They check exclusion lists, such as the OIG LEIE and SAM.gov, to ensure providers meet eligibility requirements for federal programs [7]. This automated process keeps things moving efficiently while maintaining compliance.
sbb-itb-535baee
How to Reduce Credentialing Time from 120 Days to 30
Cutting down credentialing time from 120 days to just 30 requires a focused reworking of current workflows and the smart use of technology.
Step 1: Evaluate and Map Out Current Processes
Start by breaking down your credentialing process step by step. Identify where delays occur, which tasks consume the most resources, and where inefficiencies lie. For many hospitals, inconsistent data sources across systems are a major hurdle. AI models thrive on clean, structured, and labeled data, so understanding your current data landscape is critical. Map out all your data sources and formats to prepare for smoother AI integration later.
Step 2: Standardize Data and Policies
Create a standardized provider data model and bring your policies in line with NCQA, CMS, and HIPAA requirements. Consistency in data fields and naming conventions allows AI to process information with minimal need for manual corrections. This step lays the foundation for automation.
Step 3: Implement AI-Driven Automation
Introduce AI tools in areas where they can make the biggest impact, such as data entry and primary source verification. Choose systems that are easy to use, include compliance tracking, and integrate seamlessly with existing workflows. These tools can identify discrepancies, suggest decisions based on historical data, and ensure policies are adhered to.
Step 4: Integrate AI with Existing Systems
Connect AI solutions to your HR systems, EHRs, and insurance platforms to eliminate repetitive manual tasks. Ensure these systems meet HIPAA requirements by utilizing strong encryption, multi-factor authentication, and real-time monitoring. Integration reduces redundancy and boosts efficiency across the board.
Step 5: Track, Refine, and Expand
Use dashboards to monitor progress, identify bottlenecks, and measure your return on investment. Analyze the data to fine-tune workflows - adjust templates, reorder verification steps, or address new challenges as they arise. Once the system is running efficiently, scale automation to cover additional provider types, ensuring that quality and safety standards remain intact. This continuous improvement approach not only speeds up credentialing but also ensures long-term reliability and compliance.
Maintaining Quality, Safety, and Compliance with AI
As credentialing processes become faster, ensuring quality, safety, and compliance remains a top priority. Speed without precision can jeopardize patient safety and disrupt operations. AI-powered credentialing systems strike a balance by enhancing accuracy while significantly reducing processing times. For instance, in 2025, Medallion's AI-driven credentialing system achieved a 95% success rate in credentialing audits [3].
Human Oversight and AI Governance
While AI can handle repetitive tasks efficiently, human oversight is still essential. Healthcare organizations are ultimately responsible for verifying that providers are thoroughly vetted and approved. A "human-in-the-loop" approach works well here - AI can flag issues like expired licenses, missing documents, or potential fraud, but final approvals rest with human reviewers. To maintain high standards, organizations should implement a quality improvement framework that includes regular file audits, productivity assessments, and annual policy reviews. This combination of human oversight and automated processes ensures not only efficiency but also strict regulatory compliance.
Regulatory and Privacy Requirements
AI systems in healthcare must adhere to stringent regulations. HIPAA compliance is non-negotiable, requiring encryption, multi-factor authentication, and real-time monitoring to safeguard sensitive provider data [1] [9]. These tools should only access the minimum Protected Health Information (PHI) necessary for their tasks [8]. Additionally, systems must track compliance with The Joint Commission, NCQA, and CMS standards, updating in real-time to reflect any changes. Regularly refreshing training data is crucial to prevent biases and maintain accuracy [9].
Measuring Quality Outcomes
To evaluate the effectiveness of AI in credentialing, key metrics such as error rates, provider satisfaction, and audit outcomes should be tracked. AI systems excel at spotting inconsistencies and errors that might slip through manual reviews [9]. Dashboards that display flagged exceptions, credentialing timelines, and ROI offer valuable insights. By continuously monitoring AI performance and incorporating feedback, organizations can make timely adjustments to enhance both efficiency and accuracy. These practices ensure that faster credentialing processes do not compromise the high standards necessary for optimal outcomes.
Conclusion
Cutting provider credentialing timelines from 120 days to just 30 days turns a lengthy, outdated process into an efficient system that gets providers ready to care for patients faster. By using AI-driven automation, manual tasks like data entry and document verification are replaced with digital workflows. These systems can cross-check databases, flag inconsistencies instantly, and alert teams about missing or outdated documents. This reduces human error while staying compliant with federal, state, and accreditation standards [1][4].
This streamlined process strikes a balance between speed, quality, and compliance by blending AI efficiency with human oversight. While automation handles repetitive tasks like verification and compliance checks, human reviewers step in to make final decisions and resolve flagged issues. This collaboration allows healthcare organizations to onboard providers much faster [1].
Organizations relying solely on manual credentialing face delays, higher error rates, and compliance risks that can hinder patient access to care. With AI-powered solutions proving their ability to cut credentialing times, healthcare leaders are presented with a clear path forward. These tools not only accelerate provider onboarding but also reduce administrative burdens and improve accuracy through continuous validation and monitoring.
For those ready to upgrade their credentialing process, Censinet RiskOps™ offers an all-in-one platform designed to simplify risk management and compliance. Powered by Censinet AI™, the platform uses human-guided automation to speed up assessments while maintaining essential oversight. This "human-in-the-loop" approach ensures automation supports the expertise of compliance teams, helping organizations manage risk effectively while prioritizing patient safety and care delivery.
FAQs
How does AI ensure compliance and accuracy during provider credentialing?
AI plays a crucial role in maintaining compliance and accuracy during provider credentialing. By cross-checking information from multiple trusted sources in real time, it verifies details and highlights any inconsistencies. It also keeps an eye on credential expiration dates, ensuring timely updates, and generates comprehensive compliance reports that align with federal, state, and accreditation requirements.
With advanced automation, AI significantly reduces the chances of human error. It continuously updates credentialing data, validates information, and uses risk scoring to flag potential issues early. This approach ensures provider credentials stay accurate, up-to-date, and compliant throughout the entire credentialing process.
How does AI help solve common challenges in provider credentialing?
AI is transforming the provider credentialing process by tackling common hurdles like manual mistakes, lengthy workflows, and compliance challenges. Tasks such as document verification, compliance checks, and data validation - traditionally prone to human error - are now handled through automation.
With improved data collection and real-time monitoring, AI not only speeds up the process but also ensures greater accuracy. In fact, healthcare organizations can now shorten the credentialing timeline from 120 days to just 30 days, all while maintaining high standards of quality and compliance.
How can healthcare organizations seamlessly integrate AI into their current systems?
Healthcare organizations can bring AI into their current systems by leveraging secure APIs, real-time data syncing, and reliable data exchange protocols. These tools enable AI to seamlessly interact with electronic health records (EHRs), licensing databases, and credentialing management platforms, automating tasks such as document verification and compliance checks.
By prioritizing compatibility and enforcing stringent security measures, AI solutions can simplify workflows, cut down on manual labor, and enhance precision - all while staying within regulatory guidelines. This approach allows healthcare providers to save both time and resources without sacrificing quality or compliance.


