AI in Risk Prioritization for Clinical Applications
Post Summary
AI in risk prioritization uses machine learning and predictive analytics to identify, assess, and rank clinical risks, enabling faster and more accurate decision-making.
AI improves patient safety, enhances operational efficiency, and enables real-time responses to critical risks, such as sepsis or cardiac events.
Benefits include real-time risk assessments, predictive analytics for early interventions, and improved resource allocation for high-risk cases.
Challenges include algorithmic bias, data quality issues, regulatory compliance, and the risk of over-reliance on AI systems.
Best practices include using human-in-the-loop workflows, conducting regular audits, ensuring data diversity, and establishing governance frameworks.
AI analyzes streaming data from devices and EHRs to provide continuous updates on patient conditions, enabling rapid responses to critical risks.
AI is transforming how healthcare manages risks, moving from outdated methods to smarter, faster systems. Here's what's happening:
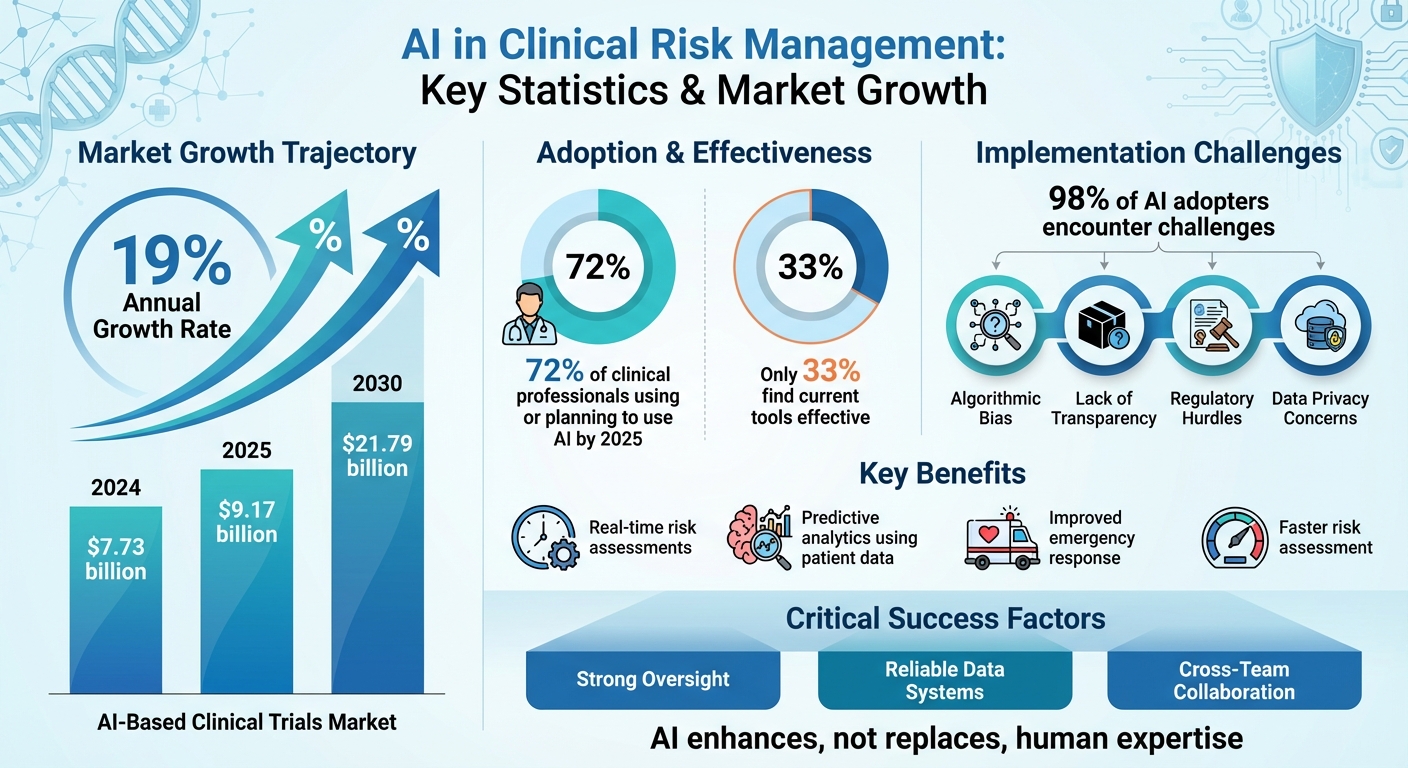
- Market Growth: The AI-based clinical trials market is projected to grow from $7.73 billion in 2024 to $9.17 billion in 2025, and hit $21.79 billion by 2030, with a 19% annual growth rate.
- Adoption Rates: 72% of clinical professionals are using or planning to use AI by 2025, but only 33% find their current tools effective.
- Key Benefits: AI enables real-time risk assessments, predicts risks using patient data, and improves responses to emergencies like cardiac arrests or strokes.
- Challenges: Issues like algorithmic bias, lack of transparency, and regulatory hurdles remain critical barriers.
AI tools, like Censinet RiskOps™, are already helping healthcare organizations assess risks faster, protect patient data, and improve decision-making. However, success depends on strong oversight, reliable data systems, and collaboration across teams. AI is not a replacement for human expertise but a tool to make healthcare safer and more efficient.
AI in Clinical Risk Management: Market Growth, Adoption Rates, and Key Statistics 2024-2030
How AI Improves Risk Prioritization in Clinical Applications
AI is revolutionizing risk prioritization in healthcare by processing massive and intricate datasets that traditional methods struggle to handle. Machine learning models analyze sources like electronic health records, device telemetry, imaging data, and clinical trial information to detect non-linear risk patterns that human reviewers might overlook. These models evolve with new data, ensuring risk scores remain relevant as conditions change.
This shift from periodic manual reviews to dynamic, ongoing risk assessment marks a major advancement in protecting both patients and healthcare operations. While traditional methods might identify risks during quarterly audits, AI systems provide real-time reassessments, ensuring resources are directed toward the most pressing issues. This is especially critical in the U.S., where healthcare organizations balance improving outcomes with managing costs. Below, we explore how predictive analytics and real-time assessments drive these advancements.
AI in Predictive Analytics for Clinical Risks
Machine learning models excel at predicting adverse events by integrating both historical and real-time data, such as vital signs, lab results, medication histories, clinical notes, and staffing levels. These models assign individual risk scores, enabling early interventions before issues escalate. For instance, U.S. hospitals utilize models trained on millions of patient records to identify high-risk patients by analyzing factors like age, comorbidities, recent procedures, and device readings.
The same predictive capabilities extend to clinical trial operations. AI models help sponsors anticipate and address challenges like protocol deviations, enrollment shortfalls, and site performance issues. By focusing oversight resources on high-risk sites, data anomalies, and safety signals, these systems streamline trial management and enhance safety monitoring without spreading attention too thinly across all activities.
AI also plays a critical role in safeguarding patient data. For data protection, AI-powered anomaly detection systems learn typical patterns of access to electronic health records and clinical applications. These models flag irregular behaviors - such as unusual login times, unexpected cross-department data access, or spikes in record access - that may indicate insider misuse or external breaches. This automation is essential for monitoring the vast access logs generated by large healthcare systems, where manual oversight would be impractical.
Real-Time Risk Assessment and Decision Support
Real-time risk assessment leverages streaming data from bedside monitors, wearables, imaging systems, and lab interfaces to continuously update risk scores. AI platforms analyze this data instantly, identifying early warning signs like arrhythmias, hypoxia, or subtle imaging changes that demand immediate attention. Care teams are alerted through EHRs, mobile apps, or centralized command centers, enabling rapid responses to both clinical and technology-related risks, such as application slowdowns that might delay critical tasks.
AI-based triage systems further enhance efficiency by ranking alerts and cases based on severity and urgency. For example, in imaging workflows, AI can prioritize studies with suspected critical findings - like intracranial hemorrhage or pulmonary embolism - at the top of radiologists' worklists. This reduces reporting times for life-threatening conditions while minimizing low-priority alerts that contribute to clinician fatigue.
For healthcare organizations managing third-party and vendor risks, AI-driven platforms like Censinet RiskOps™ offer centralized tools to assess and prioritize vulnerabilities. These platforms collect evidence, benchmark cybersecurity, and score risks based on their potential impact on patient data, protected health information (PHI), and critical workflows. By focusing on vendors whose failures pose the greatest threats to operations, healthcare organizations can better safeguard patient safety and care continuity.
Recent Research Findings
Recent studies highlight how AI has transitioned from being experimental to becoming a key component in clinical risk management. A 2025 survey revealed that 98% of AI adopters encounter challenges, particularly in areas like regulatory compliance and data privacy concerns[2]. Meanwhile, the AI-based Clinical Trials Market is expected to grow significantly - from $7.73 billion in 2024 to $9.17 billion in 2025, and further to $21.79 billion by 2030, with a compound annual growth rate of 19%[3]. These trends underscore the expanding role of AI in clinical trials and early threat detection, which are explored in detail below.
AI in Clinical Trial Risk Management
AI is reshaping how sponsors manage risks across the entire trial process. By using machine learning models, researchers can simulate trial scenarios to refine protocols before implementation, reducing the chances of failure and improving success rates. These systems combine historical data with real-time inputs to predict outcomes, allocate resources more effectively, and flag compliance issues before they lead to regulatory setbacks[3].
Novartis offers a compelling example of this transformation. In 2025, the company used AI to streamline trial feasibility assessments and site selection, automating tasks that previously required extensive manual effort. For autoimmune disease studies, Novartis employed AI-driven simulations to create adaptive protocols. These protocols adjusted doses dynamically based on patient responses, leading to faster regulatory approvals and reduced risks for patients through more personalized treatment plans[3].
AI also plays a critical role in monitoring patient adherence during trials. By identifying missed doses or protocol violations in real time, these systems help ensure safety and data integrity. Real-time alerts for adverse events enable swift clinical interventions, preventing complications from escalating. By the end of 2025, experts predict that AI will evolve from supporting isolated tasks to becoming a foundational infrastructure. For example, AI systems could automatically generate study calendars from protocols, reducing planning errors and speeding up trial timelines[4].
AI Applications in Early Threat Detection
Beyond trial management, AI excels at identifying clinical threats early. Models trained on vast datasets can detect subtle warning signs - such as early indicators of sepsis or potential medication errors - that might go unnoticed during routine evaluations. By analyzing patterns in vital signs, lab results, and medication orders, these systems flag anomalies that demand immediate attention[5].
AI’s predictive capabilities extend to operational risks as well. For instance, AI-powered dispatch systems can prioritize urgent cases like cardiac arrest or stroke by detecting nuanced communication cues and clinical details, significantly improving response times for critical conditions. A review published in Nature Digital Medicine explored AI methods for clinical trial risk assessment, summarizing existing strategies for identifying and mitigating trial-specific risks[7].
While AI enhances efficiency through real-time monitoring and adaptive designs, successful implementation depends on having interoperable data systems, strategies to address bias, and strong compliance frameworks[2]. These elements are crucial for ensuring that AI delivers on its promise of transforming clinical research and patient care.
Applications of Censinet AI™ in Risk Prioritization

Censinet AI™ leverages advanced real-time risk assessment capabilities to create practical solutions for healthcare organizations. Through its Censinet RiskOps™ platform, the company streamlines risk assessments and promotes collaboration across clinical applications, medical devices, and vendor networks.
Automated Risk Assessments and Evidence Summarization
Using machine learning, natural language processing (NLP), and rules-based engines, Censinet AI™ automates risk evaluations in areas like cybersecurity, privacy, and operations [8]. Unlike traditional manual methods, the platform processes various forms of evidence to assess risks against frameworks such as HIPAA, HITRUST, and NIST [8].
The AI engine excels at parsing complex documents - security questionnaires, SOC 2 reports, business associate agreements, penetration test results, and policy documents. It then generates concise summaries that identify key risk themes, control gaps, and actionable recommendations [8]. For example, it might produce a structured narrative like: "High likelihood of unauthorized PHI access due to lack of MFA and incomplete logging," accompanied by control maturity indicators and suggested remediation steps [8]. This automation has enabled healthcare organizations to reduce the time needed for third-party risk assessments by 70–80% compared to manual processes.
"Implementation of Censinet RiskOps™ allowed three full-time employees to be reallocated to other roles, while the remaining two FTEs were able to conduct 'a lot more risk assessments.'" – Terry Grogan, CISO at Tower Health [1]
The platform also maintains a catalog of pre-assessed vendors. When evaluating new clinical applications from existing vendors, Censinet AI™ reuses prior evidence and controls, speeding up the risk analysis process significantly [8]. For high-risk applications, the system automatically escalates cases that exceed certain thresholds - such as high residual risk scores, critical vulnerabilities, or unresolved access control issues - by generating AI-driven briefs for designated leaders [8].
Improving Collaborative Risk Management
Censinet AI™ goes beyond individual assessments by fostering a collaborative approach to risk management. The Censinet RiskOps™ platform provides a centralized, cloud-based workspace where stakeholders can access a shared risk register, assessment artifacts, and AI-generated summaries. This eliminates the inefficiencies of email- and spreadsheet-based processes [8]. Role-based access controls allow different teams - such as governance, risk, and compliance (GRC), information security, privacy, IT, and clinical engineering - to view risks through customized dashboards tailored to their priorities. For instance, clinicians can focus on patient safety, while privacy officers concentrate on compliance, and security teams monitor remediation efforts [8].
The platform acts as "air traffic control" for AI governance, directing critical findings and tasks to the appropriate stakeholders, including AI governance committees, for review and approval.
"Not only did we get rid of spreadsheets, but we have that larger community [of hospitals] to partner and work with." – James Case, VP & CISO at Baptist Health [1]
This collaborative network includes healthcare delivery organizations and over 50,000 vendors and products, enabling secure sharing of cybersecurity and risk data. This helps organizations benchmark their performance against industry standards [1].
"Benchmarking against industry standards helps us advocate for the right resources and ensures we are leading where it matters." – Brian Sterud, CIO at Faith Regional Health [1]
The platform automates comments, task assignments, and workflows, streamlining the process of negotiating risk treatments, approving exceptions, and tracking remediation. This reduces miscommunication and accelerates the deployment of critical clinical applications [8]. Additionally, when new vulnerabilities or threat advisories arise, the system quickly identifies affected vendors and applications, alerting security and clinical teams to prioritize patching and implement compensating controls before patient care is disrupted [8].
These collaborative capabilities position Censinet AI™ to tackle future challenges in AI-driven risk management effectively.
sbb-itb-535baee
Challenges in AI-Driven Risk Management and Mitigation Strategies
While earlier sections highlighted how AI can transform clinical risk management, there are still challenges that need attention to maximize its potential. Three main obstacles in AI-driven risk prioritization for clinical applications are algorithmic bias, lack of transparency, and regulatory compliance [2]. These issues can jeopardize patient safety and expose organizations to increased liability. Addressing these challenges requires a careful balance between innovation and strong oversight.
Tackling Algorithmic Bias and Improving Interpretability
Algorithmic bias occurs when AI models are trained on datasets that don't adequately represent the population. This can lead to skewed predictions that unfairly impact specific patient groups. For example, biased models might underestimate cardiovascular risks in diverse populations, leading to higher rates of morbidity [11]. According to the World Economic Forum, health AI trained on non-representative data could exclude up to 5 billion people worldwide from receiving safe and effective care [9].
One way to address this is through human-in-the-loop (HITL) oversight, where clinicians review AI outputs before making final decisions. This approach is strengthened by curating diverse datasets and conducting regular audits to identify and correct bias. Additionally, adversarial AI agents can test model outputs for consistency, and active learning systems can incorporate clinician feedback to improve accuracy over time [6].
Another critical issue is interpretability. When AI models, especially deep neural networks, fail to explain their reasoning, clinicians may lose trust in high-stakes decisions like determining trial eligibility or monitoring patient safety. Tools like SHAP (SHapley Additive exPlanations) values can help by breaking down how specific features - such as certain biomarkers - contribute to a model's risk prediction. This shifts the perception of AI from an opaque "black box" to a more transparent decision-support tool [7]. Organizations should prioritize interpretable models or use explanation tools alongside complex systems, clearly documenting their applications and limitations [7].
Navigating Regulatory and Compliance Requirements
In addition to bias and interpretability, regulatory compliance presents its own challenges. AI systems in healthcare must meet the FDA's evolving requirements for software as a medical device (SaMD). This includes documenting intended use, providing evidence of clinical performance, and establishing plans for real-world monitoring of adaptive algorithms. At the same time, HIPAA compliance demands robust data protection measures, such as de-identification, encryption, strict access controls, and detailed audit trails [3][4][8].
To meet these demands, organizations can integrate AI initiatives into their broader risk management frameworks, using standards like the NIST Cybersecurity Framework and HITRUST CSF. Healthcare-specific platforms like Censinet RiskOps™ simplify this process by centralizing vendor assessments, security evaluations, and contractual safeguards for data use and incident response [8]. Additionally, organizations should conduct threat modeling and penetration testing tailored to AI components, including data pipelines and APIs. Maintaining incident response plans that address AI-specific risks, such as model corruption or unexpected performance changes, is also critical [6][8].
"Healthcare is the most complex industry... You can't just take a tool and apply it to healthcare if it wasn't built specifically for healthcare." – Matt Christensen, Sr. Director GRC, Intermountain Health [1]
Establishing an AI oversight committee can further strengthen governance. This committee, reporting to existing quality or risk boards, should oversee the approval, monitoring, and retirement of AI tools. Importantly, licensed clinicians must retain ultimate responsibility for patient care decisions. Treating AI outputs as decision support rather than decision replacement ensures a balance between embracing innovation and maintaining accountability [4][10].
Future Directions for AI in Risk Management
AI is shifting from handling specific tasks to reshaping the very foundation of clinical operations. New advancements include automated workflow protocols, predictive analytics for trials, and ongoing monitoring in decentralized studies. With the integration of genomic data and IoT device streams, precision medicine is set to advance significantly. This integration enables real-time customization of clinical trials to align with individual genetic profiles through scenario simulations [3]. This is vital, as 59% of professionals emphasize the importance of real-time data access, yet many current systems fail to meet this need [2]. These developments pave the way for scalable applications in healthcare risk management.
Scalable AI Solutions for Healthcare Risk Management
Scaling AI in healthcare requires strong oversight to ensure safety and reliability. By using adversarial AI agents and active learning loops, systems can validate outputs and incorporate human feedback, improving both accuracy and efficiency [6]. These mechanisms allow professionals to transition from performing tasks to managing AI ecosystems while upholding safety standards.
Infrastructure is another cornerstone. Interoperable data systems are essential for integrating historical and real-time information seamlessly across teams. Raj Indupuri from eClinical Solutions highlights this as a critical element for advancing AI-driven risk strategies [2].
"Censinet RiskOps allowed 3 FTEs to go back to their real jobs! Now we do a lot more risk assessments with only 2 FTEs required." – Terry Grogan, CISO at Tower Health [1]
This example illustrates how purpose-built platforms can boost efficiency, enabling teams to handle more risk assessments with fewer resources. Looking ahead, the focus will shift to collaborative platforms that unify risk management efforts across stakeholders.
Collaborative Platforms for AI-Driven Risk Oversight
The future of AI in risk management relies on platforms that bring together stakeholders across the healthcare ecosystem. A prime example is Censinet RiskOps™, a cloud-based platform that facilitates secure sharing of cybersecurity and risk data across healthcare organizations and over 50,000 vendors and products [1]. Its Censinet AI™ capabilities streamline third-party risk assessments by auto-filling security questionnaires, summarizing vendor evidence, and generating risk reports. Importantly, these processes still include human oversight through customizable review systems [1].
This collaborative approach addresses a pressing need.
"Not only did we get rid of spreadsheets, but we have that larger community [of hospitals] to partner and work with." – James Case, VP & CISO at Baptist Health [1]
"Benchmarking against industry standards helps us advocate for the right resources and ensures we are leading where it matters." – Brian Sterud, CIO at Faith Regional Health [1]
As AI continues to evolve, these shared intelligence networks will be vital for managing the intricate risks of clinical applications. They enable organizations to collectively identify emerging threats and adapt to regulatory changes far more effectively than isolated systems ever could.
Conclusion
AI is reshaping how healthcare organizations identify and address clinical risks. By enabling continuous and proactive risk prioritization, it helps detect and mitigate threats to patient data, clinical workflows, and medical devices in real time. With the AI-based clinical trials market expected to hit $21.79 billion by 2030 and 72% of clinical professionals already incorporating AI into their work, this technology has transitioned from being experimental to becoming a core component of modern healthcare [3][2].
Solutions like Censinet RiskOps™ showcase this shift from reactive to ongoing risk management. Healthcare providers have reported measurable improvements in efficiency, completing far more risk assessments with fewer resources thanks to AI-driven automation [1]. These outcomes highlight how, when applied effectively, AI can directly enhance both operational processes and patient safety.
That said, technology alone isn’t the answer. AI should support, not replace, clinical judgment and risk management expertise [6][10]. Physicians, CISOs, and compliance teams remain responsible for the final decisions, using AI as a tool to assist their judgment. Clear escalation processes are essential for situations where AI outputs differ from clinical intuition. Platforms like Censinet RiskOps™ strike this balance by combining automation with human oversight - streamlining tasks like auto-filling security questionnaires and summarizing vendor data while leaving room for customizable review processes [1].
Looking ahead, the future of AI in healthcare will depend on interoperable data systems, rigorous AI validation against potential risks, and collaborative networks for managing threats.
"Benchmarking against industry standards helps us advocate for the right resources and ensures we are leading where it matters." – Brian Sterud, CIO at Faith Regional Health [1]
This collaborative model, which connects healthcare organizations with over 50,000 vendors through shared intelligence platforms, allows for quicker recognition of new threats and more effective responses to regulatory changes compared to working in isolation [1].
The next step combines AI-driven automation with responsible, multi-stakeholder oversight to ensure clinical applications remain safe. By deploying specialized platforms and maintaining clear accountability, healthcare leaders can harness AI as a powerful tool for delivering safer, more efficient, and more secure clinical solutions across the healthcare ecosystem.
FAQs
How does AI help reduce bias in clinical risk management?
AI plays a crucial role in minimizing bias within clinical risk management. By processing vast and diverse healthcare datasets, it can uncover disparities in decision-making and take steps to address them. This ensures that risk assessments are more balanced and equitable.
Through continuous refinement of risk models, AI keeps them accurate and aligned with fair patient outcomes. By spotting patterns of bias and fine-tuning algorithms, healthcare organizations can better prioritize risks, leading to improved clinical decisions and higher-quality care for all patients.
What are the biggest regulatory hurdles for using AI in healthcare?
AI's integration into healthcare comes with several regulatory challenges. A top priority is adhering to strict standards for patient safety, data privacy (like HIPAA), and cybersecurity. These rules are essential for safeguarding sensitive health information and preserving trust between patients and providers.
Beyond this, AI systems must also satisfy demanding criteria for transparency, explainability, and validation to secure approval from regulatory agencies such as the FDA. Proving that these tools are dependable and ethically sound is a crucial step toward their acceptance in clinical environments.
How is AI improving real-time risk assessment in clinical applications?
AI is transforming real-time risk assessment in clinical settings by processing enormous amounts of data to identify potential threats early. This allows healthcare teams to zero in on the most urgent issues, streamlining their efforts where it matters most.
With instant, data-backed insights, AI enables quicker, more informed decision-making, cutting down on delays and improving patient safety. This ensures that clinical environments can react promptly to new risks while upholding top-notch care standards.
Related Blog Posts
Key Points:
What is AI in risk prioritization for clinical applications?
Definition: AI in risk prioritization leverages machine learning and predictive analytics to identify, assess, and rank clinical risks. By analyzing vast datasets, AI systems detect patterns and assign risk scores, enabling healthcare providers to focus on the most critical issues in real time.
Why is AI important for clinical risk prioritization?
Importance:
- Enhances patient safety by identifying risks early, such as sepsis or cardiac events.
- Improves operational efficiency by streamlining workflows and reducing clinician fatigue.
- Enables real-time responses to critical risks, ensuring timely interventions.
- Supports compliance with regulatory standards by automating risk assessments and documentation.
What are the key benefits of AI in clinical risk prioritization?
Benefits:
- Real-Time Risk Assessments: AI continuously monitors patient data, providing instant updates on risk levels.
- Predictive Analytics: Machine learning models predict adverse events, enabling early interventions.
- Improved Resource Allocation: AI prioritizes high-risk cases, ensuring resources are directed where they are needed most.
- Enhanced Patient Safety: Early detection of risks reduces complications and improves outcomes.
What challenges exist in implementing AI for clinical risk prioritization?
Challenges:
- Algorithmic Bias: AI models may perpetuate biases if training data is not diverse or representative.
- Data Quality Issues: Incomplete or inaccurate data can compromise AI performance.
- Regulatory Compliance: Navigating complex regulations like HIPAA and GDPR can be challenging.
- Over-Reliance on AI: Clinicians may become overly dependent on AI systems, leading to potential errors if the system fails.
What are the best practices for implementing AI in clinical risk prioritization?
Best Practices:
- Human-in-the-Loop Workflows: Ensure clinicians validate AI outputs and provide feedback for continuous improvement.
- Regular Audits: Conduct audits to evaluate AI performance and address biases or inaccuracies.
- Data Diversity: Use diverse datasets to train AI models, reducing the risk of bias.
- Governance Frameworks: Establish clear oversight and accountability for AI systems.
- Transparency: Document AI decision-making processes to build trust among stakeholders.
How does AI enhance real-time risk assessment in clinical settings?
Enhancements:
- AI analyzes streaming data from bedside monitors, wearables, and lab systems to provide continuous updates on patient conditions.
- Early warning systems alert care teams to critical risks, such as arrhythmias or hypoxia, enabling rapid interventions.
- AI-based triage systems prioritize cases based on severity, reducing response times for life-threatening conditions.


