Food Service and Nutrition Vendor Risk in Healthcare: Safety and Regulatory Compliance
Post Summary
Healthcare organizations rely on food service vendors to provide safe and nutritious meals for vulnerable patients. However, these partnerships come with risks, including food contamination, equipment failures, and cybersecurity breaches. Poor vendor management can lead to serious consequences like patient harm, data breaches, regulatory penalties, and reputational damage.
Key Points to Know:
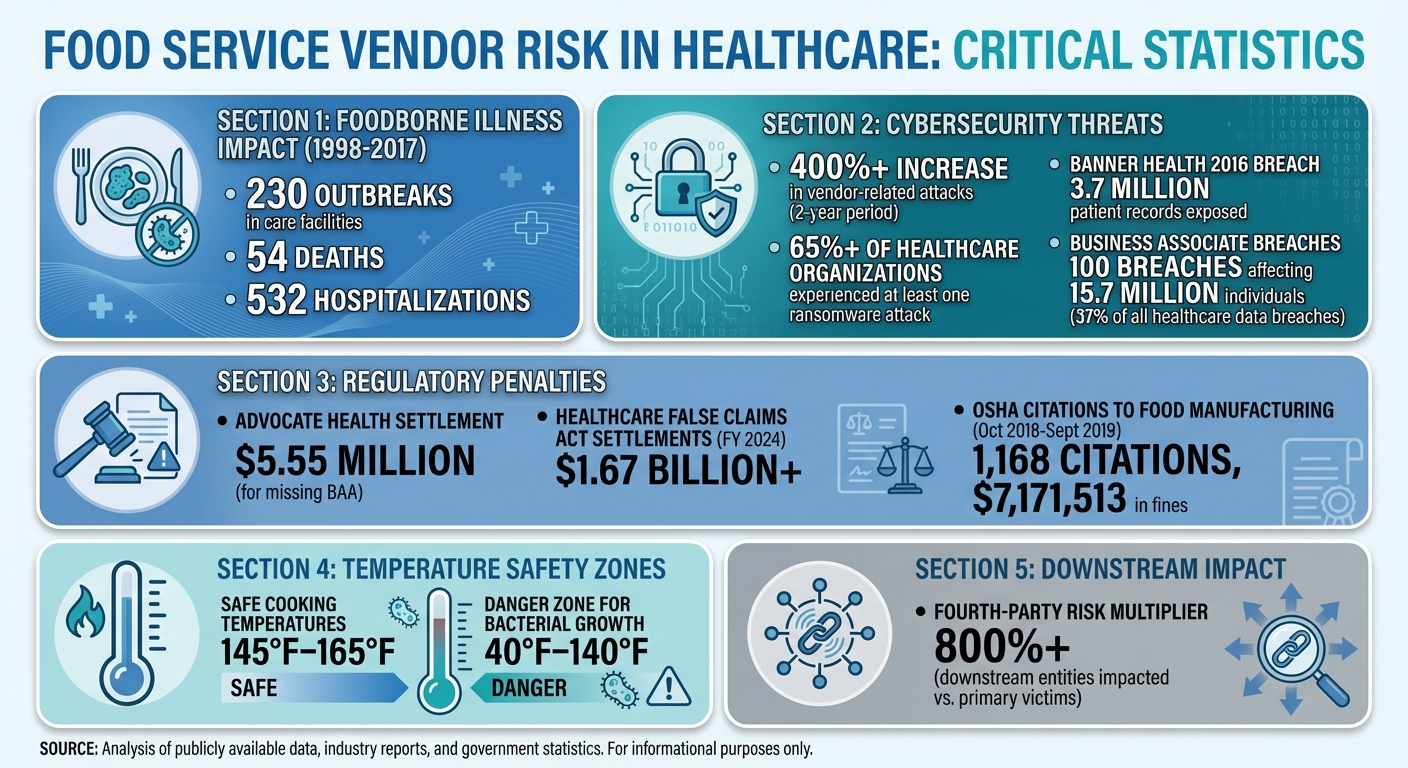
- From 1998 to 2017, 230 foodborne illness outbreaks in care facilities caused 54 deaths and 532 hospitalizations.
- Cyberattacks on vendor systems, like Banner Health’s 2016 breach, have exposed millions of patient records.
- Vendors must comply with regulations like the FDA’s Food Safety Modernization Act (FSMA) and HIPAA standards for handling patient data.
- Healthcare providers should conduct thorough risk assessments, establish Business Associate Agreements (BAAs), and monitor vendor compliance regularly.
Managing vendor risks requires diligent oversight, clear policies, and tools like Censinet RiskOps™ to centralize assessments and streamline processes. By prioritizing safety and compliance, healthcare organizations can protect patients and maintain operational integrity.
Food Service Vendor Risk Statistics in Healthcare: Key Data on Outbreaks, Breaches, and Compliance
Food Safety Risks in Healthcare Vendor Relationships
Healthcare organizations face three major food safety risks when working with food service and nutrition vendors: contamination in the supply chain, equipment and process failures, and cybersecurity vulnerabilities. These threats can endanger patient health and disrupt essential services, highlighting the importance of strict vendor oversight. Let’s dive into these categories to understand the challenges they pose.
Contamination Risks in Food Supply Chains
Food contamination can happen at any point in the supply chain. Microbiological threats like bacteria, viruses, and other pathogens are a serious concern. Physical contaminants, such as metal fragments, can enter food during processing, while chemical residues from pesticides or cleaning agents add another layer of risk [6]. Patients in healthcare settings - especially those over 65 or managing chronic conditions like diabetes or cancer - are particularly vulnerable to these hazards [8].
Equipment Failures and Process Breakdowns
Equipment malfunctions, especially around temperature control, are one of the most pressing risks. For example, undercooking food - when it doesn’t reach safe internal temperatures of 145°F–165°F - can allow harmful pathogens to survive [9]. Similarly, storing food in the "danger zone" (40°F–140°F) promotes rapid bacterial growth. Poorly maintained equipment can also harbor pathogens, and untrained employees might worsen the problem through improper handling, inadequate storage, or cross-contamination [9]. Beyond food safety, these failures can disrupt operations, cutting off critical nutrition services. For patients who rely on consistent nutritional support, such interruptions can quickly become life-threatening [1].
Cybersecurity Breaches in Vendor Systems
Digital systems play a key role in food service operations, managing inventory, monitoring temperatures, and ensuring traceability. However, these systems are increasingly targeted by cyberattacks. In fact, vendor-related attacks have surged by over 400% in just two years, with more than 65% of healthcare organizations experiencing at least one ransomware attack - often through vendor systems [1]. A cyberattack can disable temperature monitoring, corrupt inventory data, or even halt the supply chain entirely. Food service vendors, classified as "Operational Vendors" with a Medium risk level in healthcare assessments, are particularly vulnerable [2]. When critical systems fail, patients face immediate risks from service disruptions, and delayed threats from compromised food safety monitoring can be just as severe [3]. Addressing these cybersecurity gaps is critical to ensuring both food safety and uninterrupted service.
These risks emphasize the need for thorough evaluations of vendor practices to safeguard patient health and maintain operational integrity.
Regulatory Compliance Requirements for Food Service Vendors
Healthcare organizations face a maze of regulatory requirements when working with food service and nutrition vendors. These rules are designed to protect patients - especially those who are vulnerable - and ensure smooth operations. To meet these demands, healthcare providers must enforce strict standards to safeguard both patient health and their own operations.
FDA Food Safety Modernization Act (FSMA)

The FDA Food Safety Modernization Act (FSMA) shifts the focus of food safety from reaction to prevention. Instead of addressing issues after they arise, FSMA emphasizes stopping problems before they start [11]. This approach is especially critical in healthcare settings, where patients often have weakened immune systems.
Food service vendors are required to comply with specific FDA programs, such as "Preventive Controls and Sanitary Human Food Operations" and "Produce Safety Inspections" [10]. These programs mandate the use of hazard analysis protocols and preventive measures throughout food operations. In addition, healthcare providers must ensure that vendors follow the FDA's Food Code, which outlines essential standards for handling, preparing, and storing food [8][12].
HIPAA and Patient Health Information (PHI)
One often-overlooked aspect of compliance is the role food service vendors play in handling Protected Health Information (PHI). When vendors access patient dietary needs, food allergies, or billing information tied to medical records, they are classified as Business Associates (BAs) under HIPAA [14]. This designation comes with strict legal responsibilities.
To meet HIPAA requirements, healthcare organizations must establish a Business Associate Agreement (BAA) with these vendors. This agreement defines how PHI must be protected [14][16][17]. The stakes are high: in the first three quarters of 2025, business associates reported 100 breaches that impacted 15.7 million individuals, accounting for 37% of all healthcare data breaches [18].
Before working with a food service vendor, healthcare organizations should conduct detailed security evaluations, reviewing the vendor’s history with PHI, compliance measures, and overall security practices [14]. Ongoing monitoring is equally important, requiring vendors to provide auditable reports on access logs, activity, and data usage [15]. A case in point: Advocate Health faced a $5.55 million settlement after three breaches, largely due to the absence of a BAA with their vendor, Blackhawk Consulting Group. Kenneth N. Rashbaum, Partner at Barton LLP, explained:
"While it is generally accepted that any organization can be attacked - and an attack itself isn't proof of a HIPAA violation - Advocate was penalized because it failed to enter into a HIPAA Business Associate Agreement with Blackhawk. Such agreements...are a black-and-white HIPAA requirement" [18].
Joint Commission Standards for Vendor Oversight

The Joint Commission, along with the Centers for Medicare & Medicaid Services (CMS), sets standards that healthcare providers must meet to ensure patient safety and maintain quality care [19]. These accrediting bodies impose specific requirements for food and dietary services, and failing to meet them can lead to the loss of accreditation - a catastrophic outcome for any healthcare facility [19].
Organizations receiving Medicare or Medicaid funding face additional rules, including written policies covering diet manuals, therapeutic menus, meal schedules, diet orders, and tray delivery. The Joint Commission also expects compliance with regulations like OSHA's Bloodborne Pathogens regulation (1910.1030) [12]. Food service vendors are classified as "Operational Vendors" with a "Medium" risk level, meaning they must undergo regular performance audits and continuous compliance checks [2].
To maintain accreditation and protect patients, healthcare organizations need to implement quality assurance systems, conduct internal audits, and perform risk assessments to identify potential issues in vendor operations [19]. These steps are essential for meeting regulatory standards and ensuring the safety of those in their care.
Vendor Risk Assessment Methods
Healthcare organizations need a dedicated Vendor Risk Management (VRM) team to assess food service vendors effectively. This team should include representatives from executive leadership, legal, compliance, IT, and procurement departments [1]. Their role is to map out risk areas such as patient privacy, cybersecurity, physical security, data storage, and communication systems. Evaluating both the vendor and their services is critical. Organizations must prioritize vendors with strong security credentials and regulatory compliance, as cutting corners can lead to costly consequences. For example, in 2016, Banner Health faced a data breach involving 3.7 million records due to a compromised food court payment processor, resulting in significant financial and reputational damage [1]. These methods create a framework to address risks across supply chains, technology systems, and data protocols.
Supply Chain Risk Analysis
Food service vendors rely on intricate supply chains with multiple potential failure points. Healthcare organizations must assess every stage - from ingredient suppliers to transportation and storage facilities - to uncover vulnerabilities that could lead to contamination, spoilage, or security breaches. The FDA's human foods program, which uses risk analysis frameworks developed by the World Health Organization, serves as a model for prioritizing high-impact risks through science-based decision-making [20]. Adopting similar approaches ensures resources are directed where they’re needed most.
Another critical factor is fourth-party risk, which involves subcontractors that vendors rely on to deliver services. Risk reviews should include specific questions about these subcontractors. Research shows that downstream entities impacted by multi-party incidents outnumber primary victims by over 800% [21]. A breach at a subcontractor level can ripple through the supply chain, amplifying its effects. Once supply chain vulnerabilities are identified, healthcare organizations must also examine the technology and equipment used by vendors.
Technology and Equipment Risk Evaluation
Modern food service operations depend on integrated technologies for tasks like inventory management, temperature monitoring, and payment processing. However, every device or software platform connected to these systems represents a potential target for cyberattacks or operational failures. To mitigate risks, organizations should verify vendors’ adherence to cybersecurity best practices, such as implementing multi-factor authentication (MFA), following Zero Trust principles, and meeting certifications like HITRUST, SOC 2 Type 2, or ISO 27001. Physical safety protocols, such as lockout/tagout (LOTO) programs, should also be audited [22].
The importance of these evaluations is underscored by data from October 2018 to September 2019, when OSHA issued 1,168 citations to the food manufacturing industry, resulting in $7,171,513 in fines [22]. Many violations stemmed from inadequate LOTO practices, leading to severe injuries and fatalities. By carefully assessing decontamination tasks and other operational risks, organizations can reduce these dangers.
Data Classification and Protection Requirements
Classifying vendor-processed data is essential for assigning risk tiers and implementing appropriate controls, such as Business Associate Agreements for handling sensitive information [1][21]. Vendors should be categorized into general risk tiers - ranging from low to critical - based on factors like data sensitivity, system access, and the potential impact of a breach [1][21]. For instance, a vendor supplying pre-packaged meals without accessing patient data would typically be low risk, while a vendor managing therapeutic diets and sensitive patient information would fall into a high-risk category.
To ensure consistency, organizations should establish clear evaluation criteria and scoring methods for these risk tiers [21]. Standardized assessments help minimize bias and streamline the process. Periodic vendor risk assessments, adjusted for each vendor’s risk rating, are crucial for identifying emerging issues before they escalate and jeopardize patient safety or organizational stability [1][21]. By integrating findings from all these evaluation areas, the VRM team can maintain a comprehensive view of vendor risks and ensure effective mitigation strategies.
sbb-itb-535baee
Managing Vendor Risks with Censinet RiskOps™
Navigating vendor risks in today's regulatory environment demands more than just traditional assessment methods. That's where Censinet RiskOps™ steps in, offering a streamlined way to centralize risk assessments and enhance collaboration across teams. Designed specifically for healthcare organizations, this tool simplifies managing vendor risks while keeping pace with shifting regulations.
Censinet Connect™ for Third-Party Risk Assessments
Censinet Connect™ takes the complexity out of vendor risk assessments by standardizing the process. It allows organizations to conduct uniform evaluations and track responses efficiently. This consistency not only strengthens risk management strategies but also cuts down on the manual effort required, saving time and resources.
AI-Powered Risk Analysis with Censinet AI™
With Censinet AI™, risk assessments get a productivity boost. The AI quickly summarizes vendor documentation and flags critical indicators, helping teams zero in on what matters most. By automating routine tasks, it frees up risk teams to focus on key decisions, ensuring that no important detail is overlooked.
Cross-Team Collaboration with Censinet RiskOps™
Vendor risk management works best when everyone - from executive leadership to IT and procurement - operates in sync [1]. Censinet RiskOps™ bridges these departments by unifying vendor policies and workflows. It provides real-time updates on regulatory changes and emerging risks, helping organizations stay proactive in protecting both patient health and their operational integrity.
Responding to Food Service Vendor Incidents
Managing vendor-related incidents effectively is a key part of reducing risks in healthcare. Organizations are held responsible for their vendors' actions, making a quick and efficient response essential [5]. Once risks have been identified and mitigated, the focus shifts to handling incidents that arise. Whether it’s a food contamination issue or a cybersecurity breach, acting quickly safeguards both patient well-being and the organization’s reputation. The stakes are high - healthcare-related False Claims Act settlements surpassed $1.67 billion in fiscal year 2024 [13]. The initial response sets the stage for managing containment, reporting, and continuity planning.
Incident Containment and Resolution
The moment an incident is detected, containment efforts must begin. For food safety concerns, this means isolating contaminated products and stopping their distribution to prevent harm to patients. In cases of system outages, where patient safety could be at risk [1], speed is critical. Work closely with vendors to identify the root cause and put temporary measures in place. If the issue involves a data breach, activate your incident response team to secure compromised systems and prevent further exposure.
Regulatory Notification and Reporting
Once the situation is under control, notifying the appropriate regulatory bodies becomes the next priority. The requirements differ depending on the nature of the incident. For food safety, the Food Safety Modernization Act (FSMA) mandates a recall plan that includes clear steps for notifying affected parties and the public [4]. In the case of data breaches, the HITECH Act requires notification when non-encrypted health information is compromised, with significant penalties for non-compliance [13]. Business Associate Agreements with food service vendors should clearly outline HIPAA compliance responsibilities, including who is in charge of breach notifications [1][13].
Business Continuity Planning for Nutrition Services
Disruptions in nutrition services can have a direct impact on patient care, making continuity planning essential. Start by identifying and prioritizing your most critical food service vendors [23][24][2]. Evaluate each vendor’s ability to handle operational challenges, including their capacity to meet demand, logistics capabilities, and existing contingency plans [24]. Regularly test emergency communication systems, explore alternative service options, and monitor vendor performance to ensure readiness during disruptions [7][23][24][2].
Conclusion
Managing vendor risks in healthcare food services is a critical step in ensuring both patient safety and the integrity of the organization. These risks can range from physical supply chain issues to digital vulnerabilities, making it vital to address them proactively rather than waiting for problems to arise [1][2].
Strong risk management practices bring clear advantages. They enhance HIPAA compliance, minimize the chances of data breaches, streamline operations, and reduce legal exposure [1]. Most importantly, they safeguard the well-being of patients who rely on consistent and safe nutrition services during their most vulnerable times.
Healthcare organizations face unique challenges, requiring tools tailored to their specific needs. Platforms like Censinet RiskOps™ offer a centralized solution for managing third-party risks, including those tied to food service vendors. With features like Censinet Connect™ for simplified assessments and Censinet AI™ for swift risk evaluations, these tools help organizations maintain rigorous oversight without sacrificing efficiency.
The future of vendor risk management hinges on ongoing efforts - regular assessments, clear communication, strict compliance measures, and well-prepared incident response plans. Disruptions are inevitable, but organizations with strong risk management strategies can respond quickly, contain problems effectively, and ensure uninterrupted care for their patients.
As the healthcare landscape continues to evolve - with new vendors, technologies, and regulations - organizations that prioritize vendor risk management as a continuous and strategic effort will be better equipped to protect patient safety, uphold regulatory compliance, and maintain their reputation in an increasingly connected world.
FAQs
What are the biggest food safety risks when working with healthcare food service vendors?
Food safety risks in healthcare settings can pose serious dangers to patient health. Contamination from harmful pathogens like Salmonella, E. coli, and Listeria is a major concern, often stemming from issues during food preparation or storage. Temperature control is another critical factor - hot foods need to stay above 140°F, while cold foods must be kept below 40°F to prevent the growth of dangerous bacteria.
Other challenges include cross-contamination between raw and cooked foods, inadequate hand hygiene among staff, and using ingredients from unverified or unsafe sources. On top of that, failing to follow regulations such as the FDA Food Code or specific healthcare guidelines can increase risks, leading to liability concerns and compromised patient safety. Strong oversight and strict adherence to proper practices are essential to address these challenges effectively.
What is the impact of the FDA's Food Safety Modernization Act (FSMA) on food service vendors in healthcare?
The Food Safety Modernization Act (FSMA), enacted by the FDA in 2011, pushes food service vendors to adopt a proactive stance on food safety, particularly in healthcare environments. Under this legislation, vendors must develop and implement a detailed food safety plan. This plan should cover key elements such as hazard analysis, preventive controls, monitoring, corrective actions, and verification steps.
The primary goal of FSMA is to reduce the risk of foodborne illnesses by prioritizing risk-based strategies. For healthcare organizations, adhering to FSMA isn't just about meeting regulatory requirements - it’s about protecting patient health and ensuring confidence in the safety of the food supply chain.
Why is cybersecurity important for food service vendors in healthcare settings?
Cybersecurity plays a critical role for food service vendors in healthcare settings, as they frequently deal with sensitive patient and organizational data. A breach could result in exposed information, operational disruptions, regulatory fines, and, most importantly, risks to patient safety and trust.
Healthcare organizations depend on third-party vendors to uphold rigorous safety and compliance standards. Safeguarding these systems against cyber threats is essential to maintaining patient care quality, protecting the organization’s reputation, and ensuring smooth operations.


