The Automated Risk Revolution: Building AI-First Risk Management Programs
Post Summary
AI-first risk management is transforming how healthcare organizations handle cybersecurity and compliance. By automating risk detection, evaluation, and response, this approach replaces outdated manual processes, offering real-time insights and proactive threat management. Key benefits include faster risk assessments, improved accuracy, and the ability to manage complex vendor ecosystems effectively. However, successful implementation requires strong governance, high-quality data, and human oversight for critical decisions.
Highlights:
- AI in Risk Management: Automates cybersecurity threat detection and compliance monitoring, reducing errors and delays.
- Healthcare Challenges: Ransomware, data breaches, and medical device vulnerabilities demand faster, more accurate risk management.
- Core Components: Focus on patient safety, data integrity, and operational efficiency through continuous monitoring.
- Vendor Risk Management: AI simplifies onboarding, monitors risks, and ensures compliance across third- and fourth-party relationships.
- Governance is Key: Multidisciplinary oversight ensures ethical, unbiased, and safe AI use.
AI-first models are reshaping risk management, offering scalable solutions for healthcare providers while maintaining the necessary balance between automation and human judgment.
Building an AI-First Risk Management Program
Creating an AI-first risk management program goes beyond simply adopting new software - it requires a complete rethink of cybersecurity strategies. Moving past traditional approaches, this type of program redefines how risks are identified, assessed, and mitigated. The foundation of such a program rests on three main pillars: pinpointing the areas where AI can make a real difference, selecting the right technologies for specific risks, and establishing governance structures that ensure accountability. Here’s a closer look at the key elements, tech applications, and governance strategies that form the backbone of an AI-first risk management program.
Core Components of AI-Driven Risk Management
An AI-driven risk management program focuses on five interconnected areas: patient safety, data integrity, cybersecurity, regulatory compliance, and operational efficiency. By incorporating AI, organizations can shift from periodic risk reviews to continuous, predictive monitoring. This approach also facilitates ongoing third-party assessments, which are crucial for identifying vulnerabilities across the IT ecosystem. For U.S. healthcare organizations, where cybersecurity threats are on the rise, these components provide a comprehensive framework to tackle risks head-on. The potential payoff is massive - AI could help save up to $360 billion annually in the U.S. healthcare system by improving efficiency and reducing avoidable adverse outcomes [2].
How AI Technologies Apply to Risk Management
AI technologies like predictive analytics and anomaly detection are at the heart of AI-first risk management. Predictive analytics uses historical breach data and current threat intelligence to anticipate which vulnerabilities attackers are most likely to exploit. Meanwhile, anomaly detection keeps an eye on network traffic, user behavior, and system logs to spot unusual activity that could signal a security breach. These tools can catch threats that traditional, rule-based systems might overlook, making them essential for proactive risk management.
Setting Up Governance for AI Risk Programs
While AI offers tremendous potential, governance remains a major weak spot. Only 16% of health systems currently have a systemwide governance policy for AI use [2]. This lack of oversight poses serious risks - between 2022 and 2024, AI-related malpractice claims rose by 14% [4]. To address this, organizations need a cross-functional governance committee that includes data scientists, clinicians, compliance officers, and ethics experts. This committee should oversee key decisions, from project approval to system design and deployment, and ensure ongoing monitoring for issues like drift or bias.
Additionally, healthcare organizations must establish clear policies covering training data, validation techniques, and performance metrics. Without these safeguards, AI systems can unintentionally reinforce harmful biases. For example, one study revealed that a healthcare prediction algorithm was biased against Black patients. By using healthcare costs as a proxy for medical need, the algorithm flagged only 18% of Black patients for extra care, even though 47% should have qualified [2]. Proper governance can help prevent such outcomes, ensuring AI systems are both effective and equitable.
Automating Cybersecurity Risk Assessments
Automating risk assessments with AI builds on the foundation of an AI-first approach, transforming how organizations manage security. Traditional methods are often slow and prone to errors, but AI reshapes this process by automating workflows, continuously checking compliance, and delivering real-time risk scores. These platforms provide a constant view of an organization's security posture, ensuring no gaps go unnoticed [5].
Continuous Control Monitoring and Risk Scoring
AI tools work tirelessly, monitoring network traffic, user behavior, and system logs 24/7. They detect anomalies and patterns that could indicate potential threats [5]. These platforms also ensure compliance with frameworks like NIST CSF and HIPAA, identifying weaknesses and generating dynamic risk scores [1]. By consolidating risk data and breaking down silos, AI-powered analytics provide real-time insights through user-friendly dashboards. This enables faster, more informed decision-making. Additionally, predictive analytics highlight which vulnerabilities are most likely to be exploited, allowing organizations to focus their resources where they're needed most [1]. This kind of immediate insight is a stark improvement over the delays that come with manual assessments.
Manual vs. AI-Driven Risk Assessments
Manual risk assessments are slow and often riddled with errors due to human oversight. They can take weeks or even months to complete, delaying critical decisions. In contrast, AI-driven assessments operate continuously, requiring minimal human intervention. This not only reduces the time and cost involved but also significantly improves accuracy. By automating these processes, security teams can shift their focus from tedious administrative tasks to strategic initiatives that directly address risks.
How Censinet Automates Risk Assessments
Censinet RiskOps™ and Censinet AI take automation to the next level, making risk assessments faster and more efficient. Vendors can complete security questionnaires in seconds instead of days. The platform automatically compiles evidence, tracks integration details, identifies fourth-party risks, and generates detailed risk summary reports. It also validates evidence to ensure compliance requirements are met - without the need for manual review. However, the platform isn’t entirely hands-off; it incorporates human oversight for critical decision points. This blend of automation and human judgment helps healthcare organizations scale their risk management efforts without compromising safety or precision.
AI-Driven Third-Party and Supply Chain Risk Management
Third-Party Risk Challenges in Healthcare
Healthcare organizations face increasing challenges in managing vendors who handle sensitive information like Protected Health Information (PHI), medical devices, and cloud services. The situation becomes even more complex when factoring in fourth-party dependencies - those subcontractors and partners that vendors rely on. Regulatory bodies, such as the FDA, demand strict traceability within these networks to ensure compliance, while patient safety and quality standards remain top priorities [6]. Additionally, disruptions in global supplier networks often have ripple effects that can impact local operations. Traditional risk management methods struggle to keep pace with the growing number of vendors and the rapid evolution of risks. This is where AI steps in, simplifying the process by automating risk identification and management throughout the vendor lifecycle.
Automating the Third-Party Risk Lifecycle
AI platforms use natural language processing (NLP) to extract key information from complex documents like contracts, audit reports, SOC 2 certifications, and security policies. This advanced document processing speeds up vendor onboarding while categorizing vendors based on their risk levels and the type of data they access. These platforms don’t stop at intake - they continuously monitor vendor risks by analyzing factors like security posture, compliance records, and past performance. When issues arise, AI systems can automatically create remediation plans and assign tasks to the appropriate teams for resolution. This kind of automation ensures that vendor risk management programs can operate at scale. However, while AI offers speed and consistency, human oversight is still crucial for making nuanced decisions that require context and judgment.
Benefits and Limitations of AI-Driven Vendor Risk Management
AI-powered vendor risk management systems bring impressive benefits. They can process massive amounts of data in a fraction of the time it would take using traditional methods, ensuring consistent evaluations across all vendors. These systems are designed to scale, making it possible to manage hundreds - or even thousands - of vendor relationships while delivering real-time risk scoring and continuous monitoring. However, human expertise remains indispensable for critical decisions, particularly when evaluating vendors with access to sensitive patient data or systems essential to operations. It’s also important to address foundational issues like ensuring data quality, integrity, and standardization before relying on AI for accurate results [7]. The most effective strategy blends AI’s efficiency and scalability with human insight, creating a balanced and robust approach to vendor risk management.
| Advantages | Challenges |
|---|---|
| Speeds up vendor assessments, reducing timelines from weeks to seconds | Relies on high-quality, standardized data for accurate results |
| Ensures consistent evaluation across all vendors | Requires human review for critical and context-sensitive decisions |
| Scales to manage large vendor networks efficiently | |
| Detects hidden risks within fourth-party relationships | |
| Provides real-time risk scoring and continuous monitoring |
sbb-itb-535baee
Ensuring Safe and Responsible AI Automation in Healthcare
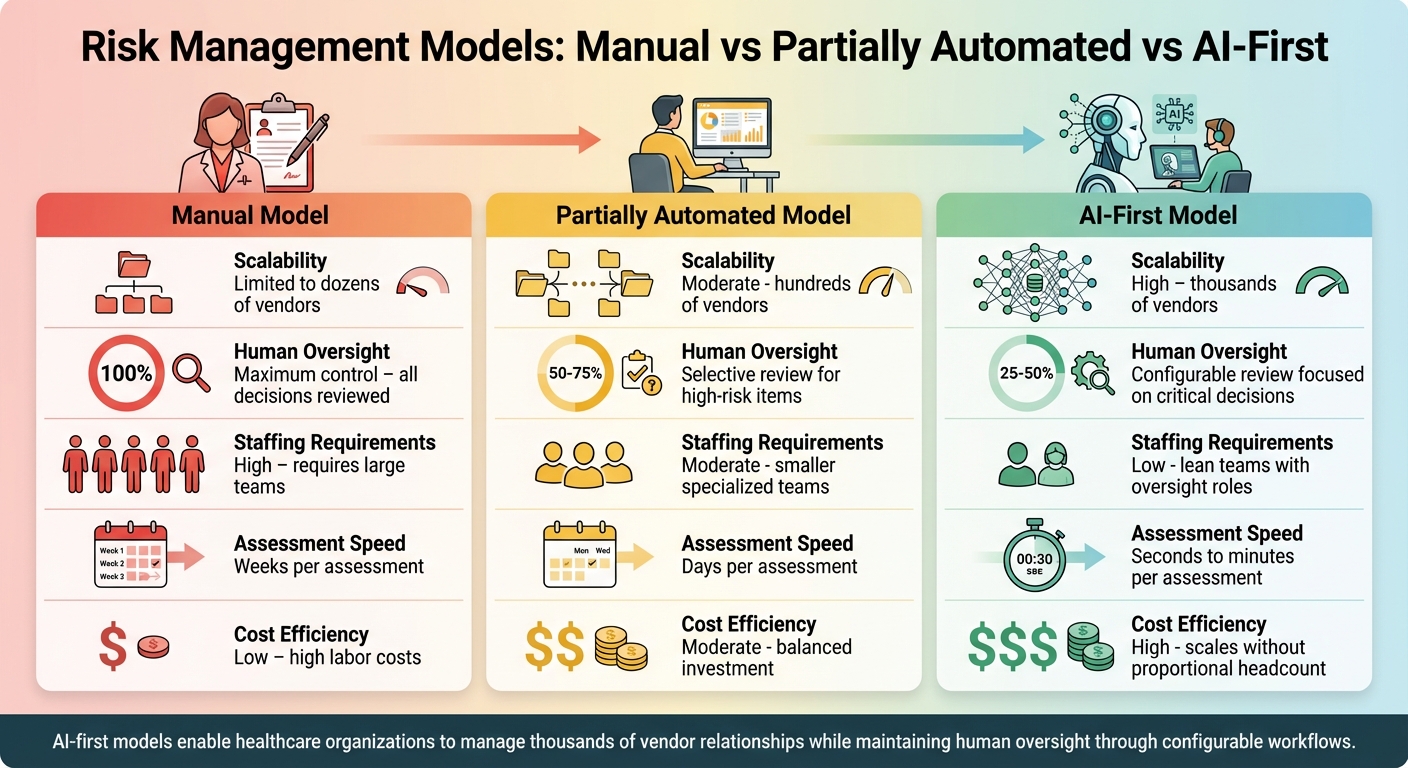
Manual vs Partially Automated vs AI-First Risk Management Models Comparison
Principles of Trustworthy AI
Building trust in AI for healthcare starts with a strong foundation of transparency, accountability, fairness, data quality, privacy, security, and ethical practices. Transparency involves understanding how AI systems make decisions, avoiding the "black box" issue where algorithms produce results without clear explanations. Accountability ensures there’s a clear chain of responsibility when systems fail or produce biased outcomes. Fairness is another critical element. For example, a study revealed that a healthcare prediction algorithm was biased against Black patients, identifying only 18% for additional care they needed[2]. With AI in healthcare expected to grow to $187 billion by 2030, these principles are more than just guidelines - they’re essential for safeguarding patient safety and maintaining trust[8]. Together, they form the backbone of human-guided automation to mitigate risks effectively.
Human-Guided AI Automation
AI in healthcare should act as a support system, not a replacement for human decision-making[3]. This balance ensures human oversight is maintained, reducing errors while benefiting from the efficiency AI offers. A well-designed system includes configurable workflows, where critical decisions - especially those involving sensitive patient information or high-risk vendors - are directed to the appropriate stakeholders for review. For instance, Censinet AI routes key findings to governance members, creating a balance between automation and human judgment. Real-time dashboards add another layer of control, offering clear visibility into AI policies and risks. This ensures that the right teams address the right issues at the right time.
Comparing Risk Management Models: Manual, Partially Automated, and AI-First
Risk management in healthcare can take several forms, each with its own strengths and limitations. Manual processes offer the highest level of human control but struggle to scale, often taking weeks to complete vendor assessments and requiring large teams. Partially automated systems strike a middle ground, blending technology with human workflows. These systems reduce assessment times to days while retaining oversight for critical decisions. On the other hand, AI-first models, like those powered by Censinet AI, complete assessments in seconds. They maintain human oversight through configurable rules and review processes, allowing healthcare organizations to manage thousands of vendor relationships without needing to expand their teams significantly. However, success with AI-first models depends on robust data quality and governance frameworks to ensure accuracy.
| Model | Scalability | Human Oversight | Staffing Requirements | Assessment Speed | Cost Efficiency |
|---|---|---|---|---|---|
| Manual | Limited to dozens of vendors | Maximum control with all decisions reviewed | High - requires large teams | Weeks per assessment | Low - high labor costs |
| Partially Automated | Moderate - hundreds of vendors | Selective review for high-risk items | Moderate - smaller specialized teams | Days per assessment | Moderate - balanced investment |
| AI-First | High - thousands of vendors | Configurable review focused on critical decisions | Low - lean teams with oversight roles | Seconds to minutes per assessment | High - scales without proportional headcount |
Implementing AI-First Risk Management in U.S. Healthcare
Key Takeaways
AI-first risk management is reshaping how healthcare organizations handle cybersecurity and vendor oversight. By replacing manual processes with AI-powered automation, healthcare providers can efficiently manage thousands of vendor relationships while keeping human oversight intact through customizable workflows. This shift is especially critical given that 50% of compliance professionals cite limited financial resources as their biggest hurdle[12][13].
The benefits go far beyond just saving time. AI-first models help organizations stay compliant with evolving regulations like HIPAA and the FDA's Section 524B guidance, boost patient safety by identifying threats faster, and reduce the staggering average breach cost of $7.42 million that healthcare organizations currently face[14]. With nearly 75% of U.S. healthcare compliance professionals already using or considering AI for compliance tasks, this technology has moved from being experimental to becoming essential[12][13].
Phased Roadmap for Implementation
To fully realize the benefits of AI-first risk management, healthcare organizations should adopt a phased approach rather than rushing into a complete overhaul. Here’s how to break it down:
- Start with a maturity assessment. Evaluate your current risk management systems, data quality, and governance structures. This step lays the groundwork to ensure your organization is ready for AI deployment[9][10]. Build a strong strategic foundation and assemble skilled teams to guide the process.
- Define success metrics and run parallel testing. Before going live, conduct pilot programs where AI assessments run alongside existing processes. Focus initial efforts on lower-risk areas like revenue cycle compliance, allowing your team to validate accuracy and build confidence in the system before expanding into more critical areas like clinical decision-making[14].
- Move to validation and deployment. Align your AI initiatives with HIPAA, FDA, and HHS requirements from the start. By April 3, 2026, HHS mandates that healthcare organizations implement minimum risk management practices, including bias mitigation, outcome monitoring, security controls, and human oversight for high-impact AI applications[11]. Multidisciplinary governance is key - bring together clinicians, ethicists, compliance officers, and IT teams to ensure patient safety and regulatory compliance are balanced effectively[14].
- Scale strategically. Use a tiered approach to automation. For lower-risk areas, allow full AI autonomy, while keeping stronger human oversight for high-stakes decisions involving sensitive patient data or critical vendor relationships. Automate evidence capture for tasks like control logs, encryption tracking, and patch history, so compliance documentation is audit-ready at all times[14].
Budgeting is another critical consideration - 60% of healthcare organizations anticipate AI integration will add 10% to their annual expenses, so plan accordingly[12][13].
Finally, focus on continuous monitoring and improvement. Measure performance against your pre-defined metrics, adapt governance frameworks as regulations change, and gradually expand AI's role into additional risk domains as your organization becomes more mature in its capabilities.
FAQs
How does AI enhance risk management in healthcare organizations?
AI is reshaping risk management in healthcare by taking over essential tasks like compliance tracking and vendor evaluations. It leverages predictive analytics to anticipate potential risks, employs anomaly detection to uncover weaknesses, and boosts threat detection to protect sensitive information.
By automating these processes, AI not only enhances efficiency but also minimizes human error. This ensures healthcare organizations stay compliant with regulations while reinforcing their cybersecurity and overall risk management strategies.
What kind of governance is needed to implement AI-driven risk management in healthcare?
To make AI-driven risk management work effectively, healthcare organizations must establish a solid governance framework that prioritizes accountability, clarity, and regulatory compliance. A key step in this process is creating an AI governance committee that includes representatives from essential areas such as IT security, clinical operations, compliance, and risk management.
This framework should be guided by well-defined policies that detail roles, responsibilities, and ethical guidelines for AI use. These policies should emphasize clarity and explainability, ensuring compliance with regulations like HIPAA. Additionally, organizations should implement regular audits, set up systems for incident reporting, and provide ongoing training for staff. These measures are vital for addressing emerging AI risks and maintaining trust throughout the organization.
How does AI help manage third-party risks in healthcare cybersecurity?
AI is transforming third-party risk management by automating essential tasks like assessing vendor security measures and performing detailed risk evaluations. It keeps an eye on vendors in real-time, spots vulnerabilities, and applies strict access controls to reduce the risk of cyber threats.
With AI in the mix, organizations can better meet regulatory requirements, strengthen defenses against data breaches, and simplify vendor risk management processes. For healthcare providers, this means they can concentrate on delivering high-quality care while keeping their cybersecurity defenses strong.


